How to maintain Adequate Milk Supply After Resuming Work ? Expert Advice
Are you looking for effective ways to maintain milk supply while resuming back to work? We are here to Support you!
There are numerous gentle ways to support your milk supply — one of them is using a breast pump regularly and effectively, which can help you continue exclusive breastfeeding for the first six months.
If the supply is dropping, increase pumping during the work day, and increase feedings at the breasts during evening, night, and early morning.
Other factors that influence the frequency and the amount of time expressing breast milk include the mother’s age, supplementation, skills and efficiency at breastmilk expression, and the type of breast pump.
The appropriate use of breast pumps may be a means to maintain milk supply and help mothers to achieve 6 months of exclusive breastfeeding. If mothers notice their supply dropping after returning to work, they should increase their pumping during the workday and increase feedings at the breast during the evening, night, and early morning.
New Families should be informed not to feed the infant in the hour preceding the mother’s return from work so that she may feed the infant at the breast soon after arrival at the center or on arrival at home.
Breastfeeding Fact: Pumping depends on – baby’s age, the need of frequency for milk expression.
Mothers also must decide if they will use a bottle or other device, such as a cup, to feed expressed milk to the baby. In either case, practice with the new method should commence before the mother’s return to work.
However, it is recommended that bottles not be introduced before the mother’s milk is well established (i.e, when the child reaches 3–4 weeks of age)
As a general rule, the earlier in the postpartum period the mother returns to full-time work, the more frequently she will need to express or pump her breasts.
The major reasons for expressing milk at work are to give the baby human milk feedings in the mother’s absence and to maintain the mother’s milk supply. The mother is also protecting her baby from infections and allergies by continuing to feed her breast milk.
Last, painful engorgement contributes to embarrassing leaking, an increased risk of mastitis from milk stasis. We don’t want that to happen to you, dear mama.
A pumping plan may work wonders for you.
Mothers should plan to pump at least three times during an 8-hour workday for at least 20 minutes if using a double pump. As the mother becomes adept at expressing or pumping and as her baby gets older, she may find that she can reduce the duration of each expression period or the number of pumping sessions to two and then to one per day.
How to choose the appropriate Breast Pumps for expressing breastmilk at the workplace?
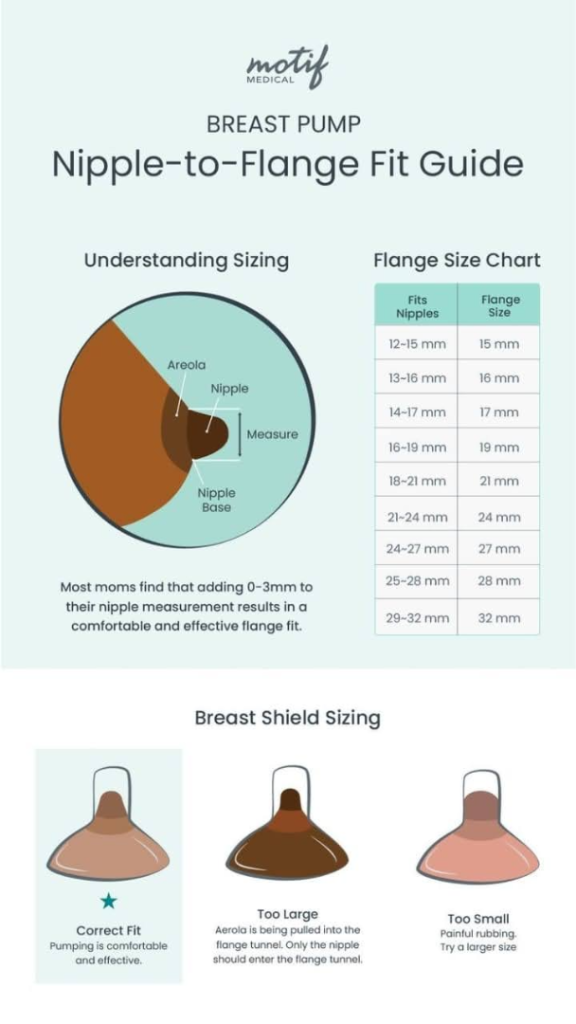
The pump should be easy and comfortable to use. Comfort depends on the closeness of fit of the pump flange on the mother’s breast, the angle of “pull” for cylinder-style pumps, and other factors.
The angle of the flange varies from one pump to another, as do the shape, size, and degree of fullness of each mother’s breasts.
Efficiency and effectiveness of the pump are factors of importance and need to be gauged based on whether the mother is comfortable with the pump during its use, whether her breasts feel softer after using the pump, and whether, over time, the amount of milk she obtains tends to increase.
Double pumping is generally more effective and efficient, and works so well with NICU babies at the Hospital setup.
Download the infographic to understand more deeply.
Real Fact: When the mother begins offering solid foods to her baby, feedings become less frequent or shorter; at that time, the amount obtained by pumping usually declines.
It’s biological, babies are not rejecting you. Let’s move on.
Most Important of all, let’s go deeper and learn about Human Milk Storage
Human milk is a dynamic substance that kills bacteria. This bactericidal ability is highest in the first several hours after expression, even when the breastmilk is not refrigerated, and some investigators have reported that colony counts remain low in such milk for at least 48 hours. Our first line of action is to feed the expressed milk first 48 hrs.
For this reason, when women use careful handwashing and clean containers in which their fresh milk is stored for less than 6 to 8 hours before refrigeration, they are not endangering their healthy babies.
Mothers who prefer to refrigerate their milk should do so in a clean, capped glass or plastic container and use the milk within 8 days after it has been refrigerated. Polyethylene bags designed for milk collection and storage are also appropriate.
However, there can be fat loss in these bags, and spillage and tearing of the bags may be issues as well.
Always use a clean container. Standard glass or plastic baby bottles (preferably bisphenol A [BPA] free), clean food storage containers with tight-fitting solid lids, and disposable feeding bottle liners. Label each container with the date and time of the earliest contribution to the container, particularly if “layering” different expressions into the same container.
Include the baby’s name for daycare center storage. Store milk in the approximate quantities that the baby is likely to need for one feeding. If refrigerated within 4–6 hours, store in a clean, tightly capped container
Milk may be stored in an insulated cooler bag with ice packs for 24 hours (39°F or 4°C). If refrigerated, use within 4–8 days. Store milk in the back of the main body of the refrigerator, where the temperature is the coolest (39°F or 4°C).
Consider storing in a separate bin or box for convenience and protection of bags. Milk can be stored in a normal refrigerator with other food items.
If frozen in a freezer maintained at −4°F or −20°C, use within 12 months.
Discard any remaining milk that was not used at the feeding for which it was thawed and warmed. Use thawed milk within 24 hours. Match the “age” of the milk as closely as possible to the baby’s age to optimize the degree of fit between the baby’s needs and the properties of the milk. Shake while thawing to remix the creamy portion that separates during storage. If a mother plans to use the milk within 8 days, it should be refrigerated rather than frozen.
If the mother finds that her milk changes in odor or consistency after storage, or if the baby begins to refuse it, she may need to reduce the storage time and freeze rather than refrigerate it to avoid possible adverse reactions.
Once the milk has been frozen, it should be either thawed quickly in a container of warm water (98°F/37°C) or thawed slowly at room temperature, monitored, and refrigerated before it is thawed completely. Milk should not be heated very quickly on a stove or in a microwave oven.
For feeding a term or older infant, milk can be fed at room temperature, body temperature, or straight from the refrigerator ( Jones, 2011). Mixing should be done not only for heat distribution but also to ensure that the creamy portion of the milk is redistributed.
Although early research indicated that the fat content of milk is altered with refrigeration and freezing, and then thawed for reuse.
Gentle swirling of the thawed milk will ensure the remixing of the fat within the milk. When giving thawed milk, the unused portion should be discarded to prevent bacterial colonization.
Re-refreezing thawed milk is not recommended. However, small amounts of fresh milk can be added to frozen milk. It is recommended that the fresh milk be refrigerated before being added to the frozen milk.
Here are the downloadable guidelines from the CDC guidelines for your deeper research, so that you can make informed and valuable decisions.
Download Here
https://www.cdc.gov/breastfeeding/breast-milk-preparation-and-storage/handling-breastmilk.html







This article is exactly what I needed! I’ve been so worried about my supply dropping once I’m back at work—thank you for these practical and encouraging tips.
hi, I am a working mother and this article is a great support for me. Thanks for your guidance.